Keeping Passion Alive: Building Grit Through Professional Development
No one in health care will disagree the last two years have been some of the most challenging of their careers. If the COVID-19 pandemic has taught us anything, it is the need for nurses and health care organizations to have grit. Lee and Duckworth define grit as a personality characteristic with two components: passion and perseverance (2018). In their view, the passion manifests as a consistency of interest over time and commitment to long-term goals, while perseverance shows as being steadfast and dedicated to working towards goals over time. Grit as a characteristic is often more predictive of success than educational attainment or innate intelligence; it is the ability to see where you want to go, create a plan and enact your plan. Grit implies a toughness of mind and character.
How do nursing leaders develop grit and resiliency in their teams? Lee and Duckworth suggest that organizations need to be both demanding and supportive. The environment needs to convey trust and safety and offer the resources for individuals to learn and grow. Encouraging and supporting our team to continue its learning and professional development is one way chief nursing officers (CNOs) and directors can instill confidence in team members, helping them to visualize and achieve goals.
Nurses are responsible for assessing their competence and ongoing professional growth. Being and feeling competent in practice affects self-respect, self-esteem and seeing the meaning of your work (Fowler, 2015). In a metasynthesis of the literature, nurses reported that continuous professional development raises professional standards and improves performance, clinical effectiveness and competence. It’s also a tool for nurses to update their skills and deliver high-quality health care (Mlambo, M., Silén, C., & McGrath, 2021). The American Nurse Association Position Statement on Professional Role Competence supports this, noting that reflective learning incorporates thoughtful personal self-assessment and analysis (2014). As leaders, how do we help nurses continue to grow in their professionalism, develop new skills, have confidence in their knowledge and advance the practice of nursing? One way to accomplish this is by engaging nurses in the process of creating their own professional development plans.
Boosting grit with professional development
In early 2021, the five Novant hospitals in the Winston-Salem area in North Carolina were dealing with the challenges of the ongoing pandemic, the loss of senior nurses to retirement as well as the loss of younger, experienced nurses who left for traveling contracts. We had just been through our largest wave to date of COVID-19 patients and leaders felt our nursing workforce was at risk of further erosion and burnout. We needed to do something that would not only help our nurses focus on their own professional development, but re-invigorate their interest in nursing practice, their own goals and remind them why they became nurses. We needed to boost their grit and support their resiliency.
Nursing leaders at Novant pulled together multiple elements to create a powerful developmental experience for our RNs. We combined:
- Reflection and the completion of a self-assessment
- A one-on-one peer review with a trusted colleague
- Creation of a professional development plan
- One-on-one structured and guided conversations with their managers
Defining the process
The first step in this journey was for each nurse to complete a self-assessment. We created a tool to guide their thinking, first asking them to reflect on their current practice, goals, strengths and opportunities. We asked them to include evidence to support their strengths (i.e., certification, clinical ladder progress, completing a degree, recognition from a patient, family or peer) and note ways that they go above and beyond their required duties (i.e., precepting students and new nurses, participation in shared governance, serving as a champion for our electronic medical record or Magnet recognition process). The next part of their self-assessment was to identify any practice changes, new skills or abilities they have gained in the last year. Finally, we asked that they reflect on opportunities and interests for their growth and development.
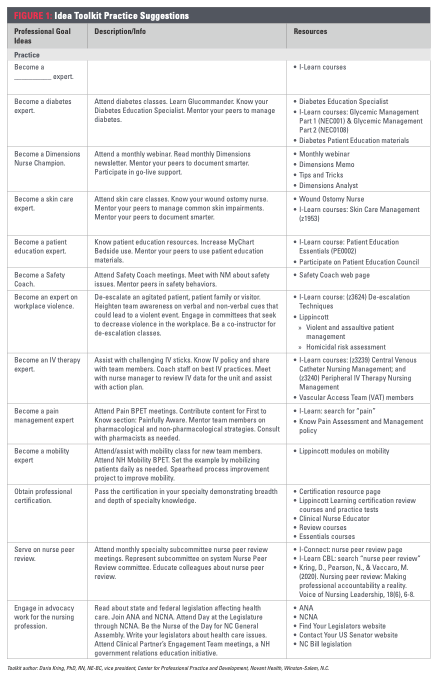
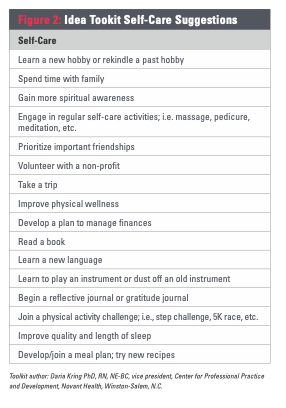
To assist nurses in contemplating what opportunities they may want to consider, our team in the Center for Professional Practice and Development created a comprehensive Idea Toolkit (See Figures 1 and 2). The toolkit covered six broad categories:
- Practice
- Education
- Research, evidence-based practice and process improvement
- Clinical leadership
- Career advancement
- Self-care
Under each category was a list of ideas, a description and the resources available. We have a wealth of resources available to support our professional development, and for ease of use, links to access the resources were embedded in the Idea Toolkit document.
We have had challenges in the past with nurses being uncomfortable with giving each other feedback directly; however, this is a hallmark of peer review and we insisted that the feedback be direct and not anonymous. Nurses could choose the peer giving them feedback in a collegial discussion. Several documents supported this process: a guide on how to give feedback, facts about what peer review is and why it is important to our profession, and a simple form to document the discussion. We approached peer review as a discussion between two colleagues, with the feedback – not the documentation – being the most important component. Therefore, the document was simple, asking for practice strengths and “did wells” and the identification of opportunities for growth. We called the document the Nursing Peer Discussion Tool, to emphasize the focus on that one-to-one, live feedback. We advised our nurses to be thoughtful in selecting who they asked to do their review, suggesting that they choose a respected colleague who had skills they wished to emulate. They could pick their best friend if they wished, but the quality of the peer review might be diminished.
Now that the nurse was armed with reflection from their self-assessment, feedback from a trusted colleague, and information from the Idea Toolkit, we asked them to complete a professional development plan. For the plan, we asked that they commit to a minimum of two goals: one for professional development and one for self-care. We asked that they include no more than four goals.
The final step in the process was a guided conversation occurring between the manager and the nurse. We created a slide deck to guide the meeting, which included a refresher of our organization’s nursing theory and practice model to help ground the discussion. The managers then reviewed several key components related to nursing practice: autonomy, nursing decision-making, shared governance and resources available to nurses to support autonomous, evidence-based practice. They reviewed avenues for information, communication and our Nursing Belief Statement and Vision.
After centering the conversation on professional nursing practice, we moved to a check-in. How were they doing? We knew that the last 18 months had been challenging and we wanted to give them a safe space to share their feelings if they wished and to offer resources as appropriate. The leaders next asked the nurse for feedback on how nursing leadership and our organization could better support them. The questions used were:
- What do you like best about your work?
- What is going well?
- What would make your job more satisfying and rewarding?
- What is your preferred method of communication and recognition?
- If you had a magic wand that could change any process on our unit, what would you change and why?
- How did you feel about giving and receiving feedback with your peers?
Finally, the manager and nurse reviewed the nurse’s professional development plan for suggestions, support and agreement.
Implementation timeline
Nursing leadership announced the implementation of the professional development plans to the nursing teams in the Winston-Salem market on May 4, 2021. The announcement was supported by FAQs, information on peer evaluation and professional development plans. The managers and directors talked through the process with their teams in huddles and staff meetings. We asked the nurses to complete the first three steps by May 31, 2021, so managers were able to begin having hour-long one-on-one meetings with their nurses on June 1. We expected some nurses would struggle to complete the first three steps by the end of May, but we wanted to allow the managers to begin so that they would have as much time as possible to have the one-on-one meetings. Our goal was for the nurse to have completed the first three steps and the managers to have met with the nurse by August 31. We wanted 75% of the nurses to complete this process by that date and 95% to be complete by Nov. 30.
To support consistency among managers with the information being shared during the one-on-one sessions, the market area CNO conducted multiple training sessions prior to the kickoff of these meetings. Guidelines for the sessions included using the slide deck mentioned earlier, having the meeting during non-work time and meeting in person if possible. The use of Zoom was allowed if both participants were in a quiet place, free from distractions.
CNOs and directors across the five hospitals were instrumental in the implementation and success of this plan. The discussion guides and supporting materials had to be created; work which was divided up among this team. Support, encouragement and mentoring of the managers was also crucial. Many of our managers have large departments with more than 100 nursing team members. Creative scheduling processes were developed to manage the logistics of having an hour-long discussion with each nurse in the span of three months.
Results
During the inaugural year, we made our goal with greater than 75% of the plans and one-on-one meetings completed by Aug. 31. By Nov. 30 over 95% of our RNs – well over 1,100 nurses – had an initial plan and had met with their manager. Feedback was overwhelmingly positive, with team members appreciating their leaders’ interest in their professional development. The one-on-one conversations helped us to focus on more than the pandemic. This year, nursing leaders in the Winston-Salem market area plan to build upon our experience in using peer feedback and discussion to create personalized development plans, further refining the process. In addition, we are expanding the process to nurses at the Novant acute care facilities in the Charlotte area. The professional development process will continue to grow our nurses’ abilities to provide meaningful, timely, appropriate feedback and further grow them professionally, strengthening their innate grit.
References
Fowler, M. (2015). Guide to the code of ethics for nurses with interpretive statements: Development, interpretation, and application. (2nd ed.). American Nurses Association.
Lee, T. & Duckworth, A. (2018). Organizational grit. Harvard Business Review. 96(5), 98-105.
Mlambo, M., Silén, C., & McGrath, C. (2021). Lifelong learning and nurses’ continuing professional development, a metasynthesis of the literature. BMC Nursing, 20(1), 62.
Professional Role Competence – ANA Position Statement 2022. https://www.nursingworld.org/practice-policy/nursing-excellence/official-position-statements/id/professional-role-competence/
About the Author

Loraine Frank-Lightfoot DNP, MBA, RN, NEA-BC, is vice president and chief nursing officer for Novant Health Forsyth Medical Center, Winston-Salem, N.C., and chief nursing officer for the Novant Winston-Salem (N.C.) market area, which includes five hospitals. Novant Health is headquartered in Winston-Salem, N.C.